Gingivitis
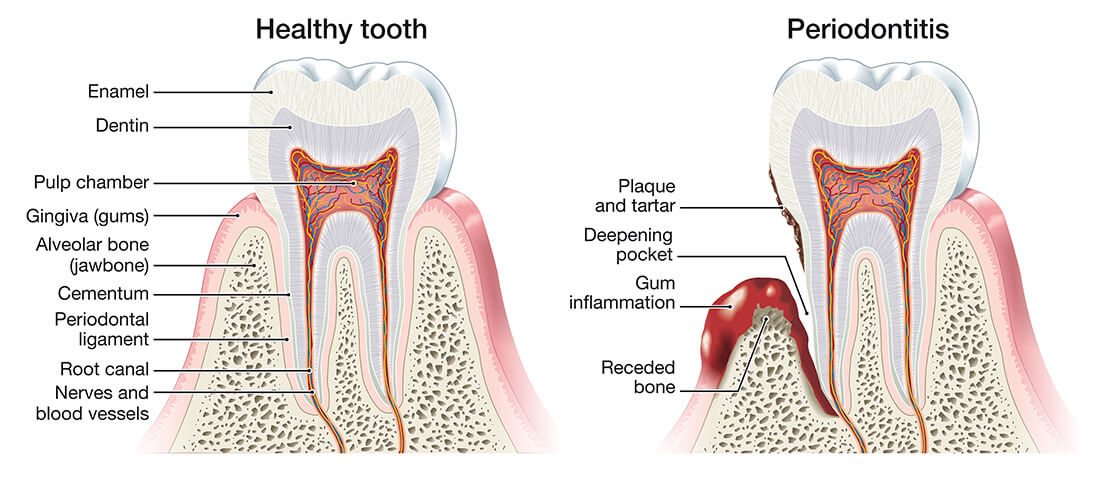
The tissues around your teeth are called the periodontium and comprise the cementum, periodontal ligament, and alveolar bone. These tissues play an essential role in the day-to-day function of your teeth and mouth, by resisting and dissipating forces created during normal oral function, such as chewing and grinding, from causing pain and discomfort. Two of the most common diseases that affect these tissues are gingivitis and periodontitis.
Periodontitis is an inflammatory condition which causes irreversible destruction of the supporting structures around your teeth. Left untreated, the damage can be so severe that your teeth end up falling out or need to be removed by a dentist. Around 25% of the population has moderate to severe forms of the disease, whilst around half of all people will experience some periodontal destruction in their lifetime.
Periodontitis is always preceded by gingivitis , although only about half of people with gingivitis develop periodontitis. Whilst gingivitis involves inflammation of your gums, periodontitis is a much more complex interaction between your immune system and the bacteria in your mouth. Put simply, the bacteria stimulates your body’s immune system to attack the supporting structures around your teeth.
This results in the formation of gingival pockets around your teeth, as the bone shrinks away faster than your gums. Left unchecked, the gingival pockets and bone loss can be so severe that your teeth become painful and need to be removed.
The signs and symptoms of gingivitis include gums that bleed during brushing, eating, and talking puffy, swollen or rounded gums that appear “angry red” painful gums.
Teeth that look long
Showing the join between the white enamel on your crown and the yellow dentine of your root
Tooth sensitivity
Food getting caught between your teeth
Bad smells from your gums and mouth
Loose teeth
You’ve noticed big changes to your bite
There are a range of risk factors which can affect the development and progression of gingivitis in your mouth, including:
Poor oral hygiene: inadequate brushing and flossing
Smoking
Dry mouth, either from medical conditions or medical treatments
Poor nutrition, including high sugar diets and diets poor in fresh vegetables
Hormonal changes
Underlying medical conditions
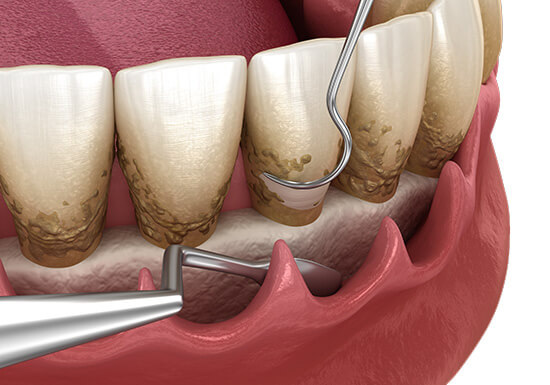
Treatment
This includes removal of the dental calculus and biofilm from your teeth and gums. This results in clean oral surfaces which can be easily maintained with appropriate at-home care.
To prevent biofilm build-up and maintain your oral health, it is important to clean your teeth and gums twice daily. Electric toothbrushes are recommended over manual toothbrushes because it improves access to those hard-to-reach teeth and surfaces in the back of your mouth. Dental floss or interdental brushes should be used to clean in between your teeth, where your toothbrush bristles can’t reach. We recommend fluoridated or sensitive type toothpastes to help harden and protect your teeth. Short-term (a couple of weeks) use of mouthwashes might be recommended to reduce your gingivitis. Occasionally we might also recommend other adjunctive products for your oral health.
Regularly having your oral health checked is important to maintain a
healthy mouth. As a minimum, you should have your teeth and gums professionally cleaned every 6 months, although in some cases your dental professional might recommend more frequent visits.
Gingivitis or Periodontitis
Hardened plaque build-up
Genetic history of periodontal disease
Rough brushing of teeth
Clenching or grinding of teeth
Misaligned teeth
While referrals are not mandatory, at The Perio Specialists, our team collaborates with your general dentist to ensure you receive specialised care and support when it comes to the management of your receding gums.
